Were You Warned? (What We Learned from the Benzo Survey)
- D E Foster
- Oct 14, 2023
- 7 min read
Welcome back to the Easing Anxiety blog series, "What We Learned from the Benzo Survey," where we dive deep into the data from the Benzodiazepine Survey of 2018/2019 to learn more about benzos, BIND, and the individuals who have taken these medications.
In our first few posts in this series, we explored age groups, gender, country, and drug type. Today, we look at a single, simple question from the survey: "Were you warned?" Were you warned about the dangers and complications associated with benzodiazepine use?
The results of the survey are quite clear on this topic, and it backs what many of us have been saying for some time.
*** Scroll to the end of this post for details about the survey and research team. ***
WERE YOU WARNED?
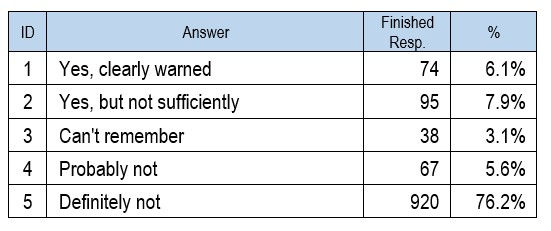
According to the survey, only 6.1% of respondents were clearly warned that benzodiazepines should be only taken for a short time, or that they are difficult to withdraw from? Another 7.9% were warned, but not sufficiently. More than 3 out of every 4 respondents (76.2%) were "definitely not warned" about the dangers of taking benzodiazepines.
Question (n=1,207):
Were you warned that benzodiazepines should only be taken for short times, or that they are difficult to withdraw from?

This data backs the anecdotal experiences shared by most of us in the benzodiazepine support field. The most common complaints many of us hear from the individuals we work with is that they were not warned or were tapered too quickly. Many even claim that they were met with annoyance, disdain, and disbelief from their own doctors.
Doctors love prescribing benzos because it's the most efficient way to get a complaining patient out of the office in the shortest possible time... 90 percent of benzo prescriptions are written, often carelessly, by primary care doctors, who can spend only seven minutes with the patient without giving serious thought to the considerable risk... — Dr. Allen Frances, Professor Emeritus at Duke University, Chairman of the DSM-IV Committee
IN THEIR OWN WORDS
This survey allowed respondents to provide additional feedback on any topic in an open-ended text box. Many of them took this opportunity to share their frustrations with the prescribing and deprescribing practices of their physicians and/or psychiatrists.
Here is a small sample of those responses:
My doctor never warned me of what benzodiazepines could do to my body. He's still trying to prescribe me more.
I had been taking .5 mg of clonazepam for 4 years, completely unaware that it was a benzo and a very dangerous drug. I wish I knew more before I began the taper a year ago, but my doctor didn't warn me, and I had no reason to research it since I've gone off of medications before without difficulty.
Am so frustrated and disappointed that we were not given correct warnings on these meds.
From my first dose on a benzodiazepine, I had adverse effects. My doctors did not recognize the medication to be the cause and actually diagnosed me with anxiety because my seizures were non-epileptic.
I wasn't warned about benzo use by my doctor until I was having difficulty discontinuing use.
My doctor cut me off without warning. They don't have a clue how to treat the after effects. Also, went to emergency room within days of being discontinued and was "locked down" in mental health unit for 9 days... Was given gabapentin, phenobarbital, and finally 5 mgs of valium once nightly during last 3 days of stay.
I went to 37 doctors looking for answers for my declining health. Even went to the Mayo Clinic. Not one doctor recognized that I had hit benzo tolerance. When I started tapering, not one recognized the withdrawal symptoms.
Asked my doctor flat out if Xanax is addictive. He said no and continued to prescribe them at increased doses for 20 years.
My doctor, a trusted psychiatrist, told me my body needed this, like a diabetic needs insulin, and promised me it was not addictive. I believed him, and never abused the RX, but hit tolerance in 2015, still struggling over 3 years later, no one has ever told me about tolerance, all Drs have told me I am mentally ill.
Doctor had no knowledge how to detox me and never warned me that lorazepam was for short-term use and kept me on it for eight years and then stopped refills he said due to FDA coming down on doctors . Pharmacist helped me detox in six month taper.
Please warn doctors to only prescribe benzos for a short period of time. No benzo should be prescribed long-term.
When I was put on Xanax my kids decided I was "nuts". This led to them throwing me and my husband out of their respective homes over time. I have no relationship with my children anymore and if something happens to my husband I really have no one — I have no reason to live. I trusted the doctor that prescribed this — he is not my doctor anymore. Unfortunately, I have had over 10 different doctors and NONE of them told me Xanax was bad!
WHAT CAN BE DONE?
The data from this survey backs what has been clear to most benzo organizers and advocates for many years; that many medical professionals are not properly educated on benzodiazepine prescribing, deprescribing, and the lasting effects of protracted withdrawal, or BIND.
The good news is that there are several organizations working towards fixing this problem.
In addition to Easing Anxiety, other groups such as the Alliance for Benzodiazepine Best Practices and Benzodiazepine Information Coalition (BIC) have made great strides in the area of medical education.
Another group —which I have had the pleasure of co-chairing for the past few years — is the Benzodiazepine Action Workgroup (BAWG). In addition to ongoing research involvement and developing the first national Peer Support Training Program specific to benzodiazepines, this group provides continuing medication education (CME) courses and evidence-based PDF documentation on prescribing, deprescribing, and peer support free and available to all on its website.
While this is a long and arduous uphill battle, progress is being made on many fronts and I personally want to thank all of those individuals who have been involved in helping improve the medical establishment's treatment of benzodiazepine-affected individuals.
References
ORGANIZATIONS
The Alliance for Benzodiazepine Best Practices — https://benzoreform.org
Benzodiazepine Action Work Group (BAWG) — https://benzoaction.org
Benzodiazepine Information Coalition (BIC) — https://benzoinfo.com
Easing Anxiety — https://easinganxiety.com
DOCUMENTATION & PROGRAMS
BAWG Guidance Documentation (Prescribing, Deprescribing, Peer Support) — https://www.easinganxiety.com/post/benzodiazepine-guidance-from-bawg
BAWG Peer Support Training Program — https://benzopeertraining.org
Benzodiazepine-Induced Neurological Dysfunction (BIND) — https://easinganxiety.com/BIND
RESOURCES
Frances, Allen. Yes, Benzos Are Bad for You. Originally published in Pro Talk: A Rehabs.com Community, June 10, 2016. Accessed October 13, 2016. https://www.psychologytoday.com/us/blog/saving-normal/201607/yes-benzos-are-bad-you.
Survey papers are listed below.
About the Benzodiazepine Survey
About the Research
The largest survey of its kind, "The Benzodiazepine Survey of 2018/2019" was created and administered by Jane Macoubrie, PhD and Christy Huff, MD. Over 1,600 individuals took the survey, resulting in 1,207 qualified respondents. The survey constituted 20 questions, including demographic inquires. Some of these questions had multiple sub-questions and/or allowed multiple answers.
The survey generated three published research papers in scientific journals (as noted below) between April 25, 2022 and June 29, 2023. The research team is still together working on new benzodiazepine-related research projects.
Special thanks to the Alliance for Benzodiazepine Best Practices for sponsoring and organizing this research.
Published Papers
PAPER 1 — April 25, 2022
Finlayson AJ, Macoubrie J, Huff C, Foster DE, Martin PR. Experiences with benzodiazepine use, tapering, and discontinuation: an Internet survey. Therapeutic Advances in Psychopharmacology. 2022;12. doi:10.1177/20451253221082386. https://journals.sagepub.com/doi/full/10.1177/20451253221082386.
PAPER 2 — February 6, 2023
Huff C, Finlayson AJR, Foster DE, Martin PR. Enduring neurological sequelae of benzodiazepine use: an Internet survey. Therapeutic Advances in Psychopharmacology. 2023;13. doi:10.1177/20451253221145561. https://journals.sagepub.com/doi/10.1177/20451253221145561.
PAPER 3 — June 29, 2023
Ritvo AD, Foster DE, Huff C, Finlayson AJR, Silvernail B, Martin PR. (2023) Long-term consequences of benzodiazepine-induced neurological dysfunction: A survey. PLOS ONE 18(6): e0285584. https://doi.org/10.1371/journal.pone.0285584.
Research Team
Research Team / Authors (alphabetical)
A. J. Reid Finlayson, MD, MMHC — Vanderbilt University Medical Center
D E Foster — Benzodiazepine Action Work Group
Christy Huff, MD — Benzodiazepine Information Coalition
Peter R. Martin, MD, MSc — Vanderbilt University Medical Center
Alexis Ritvo, MD, MPH — University of Colorado Anschutz Medical Campus
Bernard Silvernail — The Alliance for Benzodiazepine Best Practices
Acknowledgements
The Alliance for Benzodiazepine Best Practices — Sponsoring Organization
Jane Macoubrie, Ph.D. — Survey originator
Jo Ann LeQuang — Medical Writer
Limitations
This study has several limitations.
The study reported on ‘suicidal thoughts’, which can range from fleeting notions of self-harm to passive desperation, preparatory planning, and disinhibition. Suicidal thoughts may be underreported, even in an anonymous online survey, as respondents might hesitate or be embarrassed to report self-destructive thoughts.
There was no control group. Much of the survey dealt with symptoms presented in multiple-choice lists, and it is possible that patients may have been suggestible to the list presented, may not have correctly remembered past symptoms, or may incorrectly attribute certain symptoms or feelings to benzodiazepines.
We did not account for a nocebo effect.
The large number of write-in comments suggests that many respondents felt the survey did not allow them to fully describe the extent of their experiences and emotions.
Another limitation of our survey is that it recruited respondents from social media and online sources that deal with benzodiazepine use and withdrawal. Respondents were self-selected, forming a convenience sample that may not represent the population of benzodiazepine users as a whole because visitors may have sought sites such as these specifically because they have experienced problems. Moreover, those who use the Internet for health information tend to be younger, and those who join online support groups for medical conditions tend to be in generally worse health. Our results thus may not be generalizable to the population of all people taking benzodiazepines.
Data Analysis
A medical statistician produced the initial results of this survey utilizing SAS Software. Subsequent data analysis was performed in greater detail by an experienced data scientist who imported the survey data into a custom SQL Server data model.
Customized queries were employed to obtain correlations among the data. In particular, this analysis examined conditions for which benzodiazepines were prescribed and compared them to symptoms and adverse life effects reported by patients who were tapering or had discontinued benzodiazepine use.
All analyses were delivered via a structured reporting process and validated against the original SAS reports. The survey was made available online through websites and internet benzodiazepine support groups and general health and wellness groups.
The data scientist mentioned above is D E Foster, who is also the author of this blog series and the founder of Easing Anxiety. D has been a member of the Benzodiazepine Survey Research Team since 2019, providing general benzodiazepine knowledge and lived-experience in addition to formal data analysis and reporting. Prior to his withdrawal from benzodiazepines, D worked as a database developer and data scientist for over 25 years.
For Informational Purposes Only
All information presented on Easing Anxiety is for informational purposes only, and should never be considered medical or health advice. Withdrawal, tapering, or any change in dosage of benzodiazepines or any other prescription drugs should only be done under the direct supervision of a licensed physician.
This article was written by a living, breathing, human person.
Please read our site disclaimer for more information.

Commenti